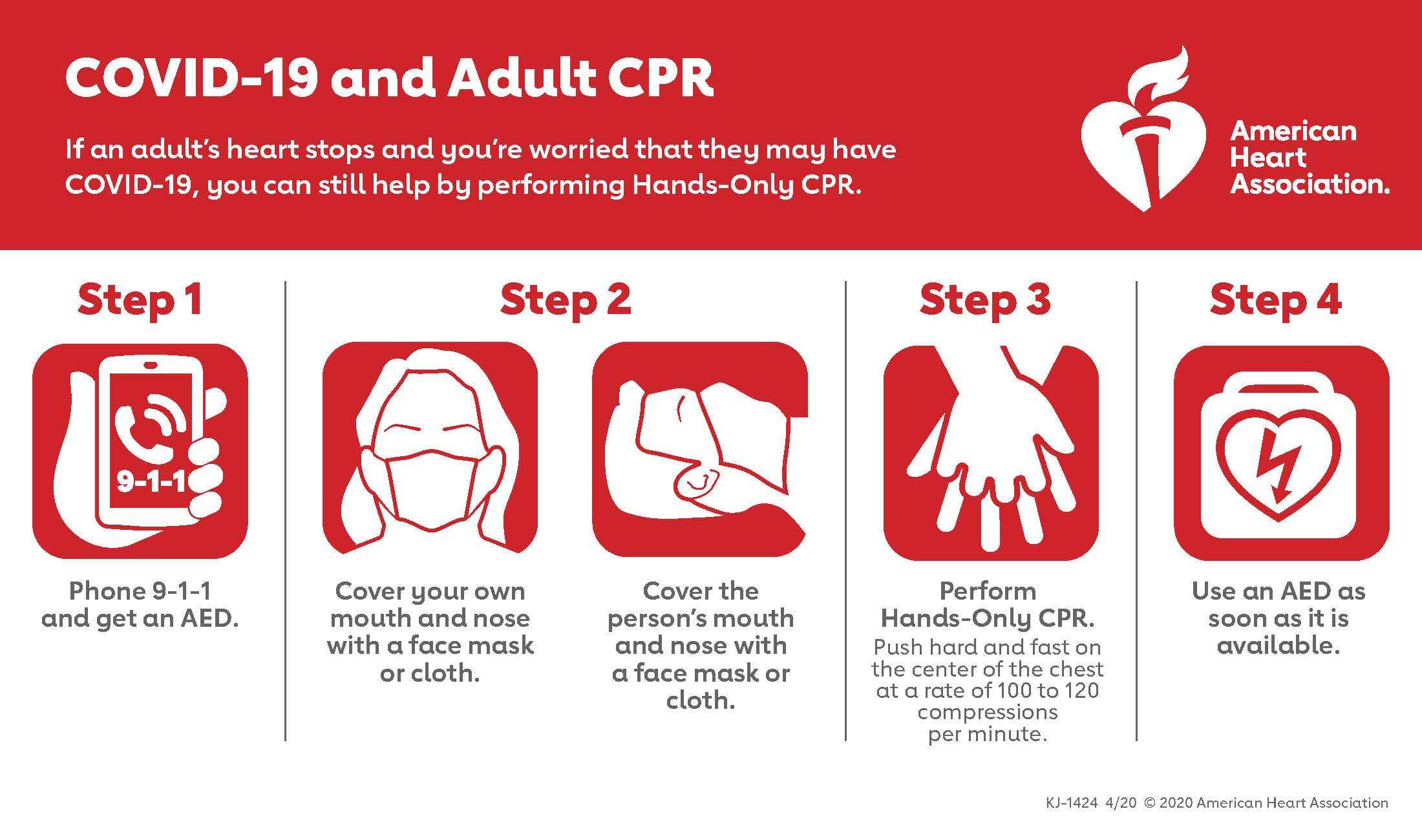
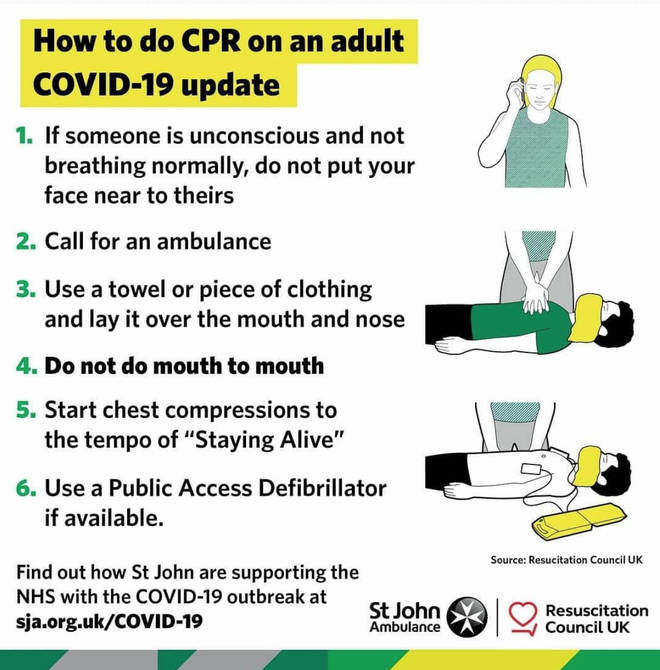
The American Heart Association (AHA) issued interim cardiopulmonary resuscitation (CPR) guidelines that apply during the COVID-19 pandemic. The AHA recommended bystanders and lay rescuers administer “hands only” CPR without mouth-to-mouth ventilation to limit exposures to the SARS-CoV-2 virus that causes COVID-19.
Those administering CPR as first aid also should consider covering their own and the cardiac arrest victim’s nose and mouth with a face mask or cloth to reduce the likelihood of disease transmission. Rescuers should use an automated external defibrillator (AED), if one is available, because defibrillation is not expected to generate aerosol particles.
The risks of infection can be even higher when administering CPR in a healthcare facility.
Healthcare workers already are at the highest risk of acquiring SARS-CoV-2, according to the AHA, and administering CPR creates additional risks:
- CPR can involve a number of aerosol-generating procedures that include performing chest compressions, providing positive-pressure ventilation, and establishing an advanced airway through intubation;
- Resuscitation can require providers to work in close proximity to one another and the patient; and
- The urgency to resuscitate a patient in cardiac arrest can result in lapses in infection-control protocols.
The AHA recommended additional precautions for emergency medical services (EMS) technicians and healthcare workers. Both EMS personnel and healthcare workers should don personal protective equipment (PPE) to guard against contact with both airborne and droplet particles before entering a patient room or scene of a cardiac arrest. Only essential personnel should be allowed in the room or on the scene.
EMS personnel and healthcare workers should protect themselves and their colleagues from unnecessary exposure to confirmed or suspected COVID-19 infections, according to the AHA.
Healthcare facilities should consider replacing manual chest compressions with mechanical CPR devices to reduce the number of rescuers required in a room. Intubation involves a high risk of aerosolization, but a closed-loop ventilation system has a lower risk of aerosolization than other ventilation methods.
Healthcare workers should use a bag mask with a tight seal and an attached high-efficiency particulate air (HEPA) filter before intubation or if intubation must be delayed. Healthcare workers also should consider using video laryngoscopy to reduce exposure to aerosolized particles during intubation.
The AHA, in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, American Society of Anesthesiologists, and Society of Critical Care Anesthesiologists, with the support of the American Association of Critical Care Nurses and National EMS Physicians, compiled the interim guidelines.
The National Safety Council (NSC) announced its support for and recommendation of the interim CPR guidelines.
Occupational Safety and Health Administration (OSHA) standards require employers to provide medical services and first aid, and some include requirements for employee training in CPR.
OSHA’s general industry medical services and first-aid standard (29 CFR 1910.151) requires that employers have personnel trained in first aid but does not contain a specific requirement for CPR training. Voluntary guidelines recommend that employers have personnel trained in providing CPR and the use of AEDs.
Other standards do have CPR training requirements. For example, the electric power generation, transmission, and distribution (1910.269); logging operations (1910.266); and permit-required confined spaces standards (1910.146) all have requirements for employee CPR training.
Article Source: https://ehsdailyadvisor.blr.com/2020/04/american-heart-association-issues-covid-19-cpr-guidelines/