Understanding the term HCP is essential for anyone in or interacting with the medical field. If you’ve ever asked, “What does HCP stand for?”, the answer is simple: HCP stands for Healthcare Personnel. This term refers to all individuals delivering health services to patients, either directly or indirectly. Whether you’re a nurse, physician, paramedic, technician, or even administrative staff in a clinical setting, you fall under the category of Healthcare Personnel. The HCP meaning goes beyond just those who provide hands-on care—it also includes individuals who support care delivery through essential roles in healthcare environments. Understanding who qualifies as an HCP is vital for correctly applying workplace policies, safety protocols, and public health guidelines. This article will explain what HCP means and why it’s a critical classification in everyday healthcare operations and emergency response planning.
HCP in Healthcare: Definition & Scope
Understanding the scope of Healthcare Personnel (HCP) helps clarify how healthcare systems function effectively. According to the CDC, HCP includes all individuals working in healthcare settings who have potential exposure to patients or infectious materials. This broad HCP definition includes those who deliver direct patient care and those who support healthcare services. With over 22 million people employed in U.S. healthcare, the sector is the nation’s largest employer, highlighting the massive scale of the healthcare workforce. Recognizing who qualifies as an HCP is essential for implementing health and safety regulations across various roles and settings.
Who qualifies as an HCP?
Knowing who falls under this category is essential when asking what HCP stands for. Healthcare Personnel include a wide range of roles. These individuals may have clinical, technical, or supportive responsibilities in healthcare environments.
Healthcare Personnel (HCPs) include many professionals who contribute to patient care and medical operations. Key groups include physicians and surgeons, registered nurses, nurse practitioners, and physician assistants (PAs) who provide direct clinical care. Therapists—such as physical, respiratory, occupational, and speech therapists—offer essential rehabilitative services. Pharmacists and pharmacy technicians ensure proper medication management, while medical and nursing assistants support daily patient care tasks. Dentists and dental hygienists focus on oral health. Laboratory and radiologic technologists handle diagnostics, and administrative and support staff maintain efficient healthcare operations. Together, they form the backbone of the healthcare workforce.
With approximately 817,920 physicians and surgeons in the U.S. as of May 2023, this group represents a significant segment of the broader HCP population.
Roles & responsibilities of HCPs
The HCP responsibilities span multiple care and support areas, ensuring the healthcare system remains functional and responsive. Preventive duties include administering vaccines, educating patients on health risks, and performing routine screenings. Curative tasks involve diagnosing illnesses, performing procedures, and managing treatment plans. Beyond clinical care, healthcare personnel are also expected to communicate, provide emotional support, and educate patients and their families about health.
Compliance is another key aspect of HCP roles. They must follow guidelines for infection control, patient confidentiality, documentation standards, and ethical medical practices. These responsibilities are critical for patient safety and public health. With over 22 million individuals in the healthcare workforce, each HCP must contribute to a consistent standard of care.
Understanding the HCP definition helps recognize the wide range of duties involved and supports better policy development, staffing strategies, and healthcare delivery outcomes.
HCP in Pharma: Engagement & Importance
Pharmaceutical companies rely heavily on Healthcare Personnel (HCPs) to advance medical knowledge, ensure safe medication use, and improve patient outcomes. Understanding what HCPs stand for in this context is vital—they include physicians, pharmacists, nurse practitioners, and others who guide how medications are prescribed, dispensed, and monitored. Effective engagement between pharmaceutical companies and healthcare workers benefits clinical practice and public health.
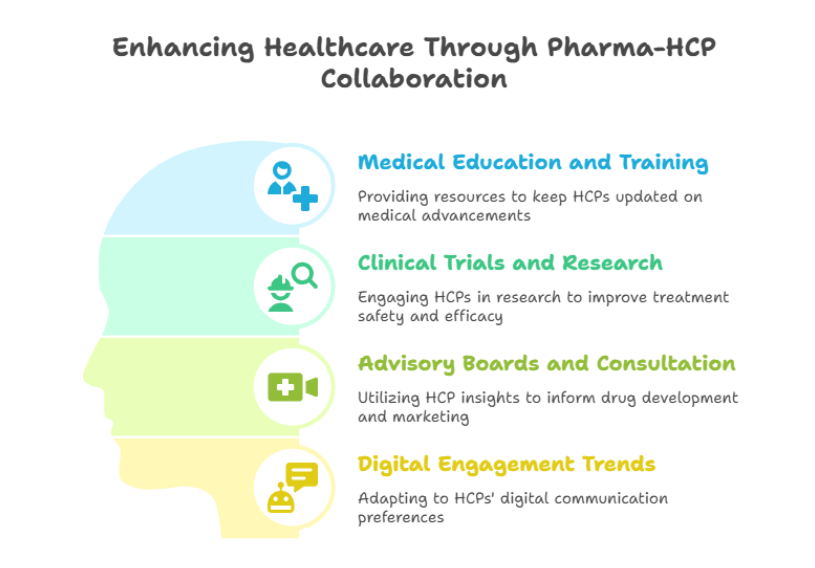
Medical education and training
Pharma companies often provide educational resources to HCPs through continuing medical education (CME) programs, webinars, and scientific materials. These initiatives ensure that Healthcare Personnel stay current on drug indications, side effects, and evolving treatment protocols. In a rapidly changing medical landscape, this kind of support helps maintain high standards of care.
Clinical trials and research collaboration
Pharmaceutical firms also engage HCPs in clinical trials to learn about the safety and efficiency of new treatments. HCPs play critical roles as investigators, coordinators, and advisors. Their insights during trial design and implementation improve study relevance and patient outcomes. This partnership is essential to the development of evidence-based treatments.
Advisory boards and consultation
HCPs are frequently invited to join advisory boards or serve as consultants. Their frontline experience helps pharma companies know patient needs, treatment barriers, and clinical workflows. These collaborations influence drug development strategies and marketing practices while keeping them grounded in real-world care environments.
Digital engagement trends
With changing communication preferences, digital channels have become key to pharma-HCP interaction. As of 2022, 63% of physicians are considered “digital omnivores”, using multiple platforms such as email, webinars, and mobile apps—up from just 31% in 2019 (Indegene Digital Savvy HCP Survey). This shift underscores the need for versatile digital engagement strategies that align with modern HCP responsibilities and work environments.
Pharma-HCP collaboration continues to play a vital role in uplifting health outcomes and shaping the future of medicine.
HCP in Other Contexts
While the term HCP is widely recognized in the healthcare industry to describe professionals such as nurses, pharmacists, and therapists, it also appears in different fields with distinct meanings. Understanding these variations is essential to avoid confusion, especially in technical discussions. Whether you’re working in materials science, information technology, or recreational activities, the acronym HCP can take on new definitions. The following sections will examine how HCP is used beyond healthcare, including in engineering, cloud services, and everyday terminology.
Hexagonal close-packed (Materials Science)
In materials science, HCP stands for hexagonal close-packed, a typical arrangement of atoms in metallic crystals. This structure is one of the most efficient atomic packing arrangements, with a packing efficiency of about 74%. It describes how atoms are densely packed in a repeating hexagonal pattern, contributing to the strength and stability of certain metals. Examples of metals with an HCP structure include titanium, magnesium, and zinc. These materials often exhibit high strength and corrosion resistance, making them valuable in aerospace, medical devices, and industrial applications.
Understanding HCP structures is essential for materials engineers and researchers developing metal alloys for specialized use. While unrelated to nurses, pharmacists, or therapists, this version of HCP plays a crucial role in manufacturing and design technologies that sometimes benefit the healthcare industry, such as surgical tools and implantable devices.
HashiCorp Cloud Platform
In cloud computing, HCP refers to the HashiCorp Cloud Platform, a managed services suite that simplifies infrastructure deployment and security. HCP enables organizations to run popular tools like Vault, Consul, and Terraform in a fully managed cloud environment. These services support consistent infrastructure management, identity protection, and service networking across cloud platforms. The platform helps IT teams deploy and scale applications securely while reducing operational overhead. Although this form of HCP operates outside the traditional healthcare industry, healthcare organizations increasingly rely on cloud-based services for electronic health records, data storage, and compliance. For nurses, pharmacists, and therapists working in modern healthcare settings, this cloud infrastructure ensures they can access secure patient data and medical tools quickly and reliably. As digital transformation grows, the HashiCorp Cloud Platform supports the broader healthcare innovation ecosystem.
Other uses
HCP also appears in everyday terms outside science and technology. In the card game bridge, HCP stands for High Card Points, a scoring method used to evaluate a player’s hand strength based on the value of face cards. In golf, Handicap is sometimes shortened to HCP, referring to the numerical measure of a player’s potential ability, helping level the playing field between competitors of different skill levels. In Australia, the Home Care Package (HCP) is a government-subsidized program that provides long-term support to older individuals who wish to remain at home. It includes personal care, domestic assistance, and nursing support tailored to each person’s needs. While these uses are unrelated to pharmacists, therapists, or nurses directly, they reflect the diverse meanings the acronym HCP can hold. In particular, the Home Care Package system closely intersects with the healthcare industry, highlighting the importance of accurate interpretation based on context.
Why Understanding HCP Matters?
Recognizing the correct meaning of HCP is essential across various professional settings—especially in the healthcare industry, where nurses, pharmacists, therapists, and other professionals work in high-stakes environments. Understanding what HCP stands for ensures consistent communication, better coordination, and improved outcomes for healthcare providers and patients.
Improved communication and coordination
In the healthcare workforce, clarity around the HCP definition supports smoother communication among multidisciplinary teams. Whether between nurses, physicians, pharmacists, or therapists, understanding who qualifies as an HCP helps define roles, responsibilities, and expectations. This clarity minimizes confusion, especially when implementing protocols, distributing tasks, or coordinating care plans.
Better compliance and safety
Accurately identifying Healthcare Personnel is also essential for legal and regulatory compliance. Guidelines from the CDC, OSHA, and other agencies often apply specifically to HCPs. This includes training requirements, infection control protocols, and vaccination mandates. Knowing who falls under this category ensures organizations meet compliance standards and keep their teams and patients safe.
Better patient outcomes
When HCP responsibilities are clearly defined, healthcare teams function more effectively. This leads to faster diagnosis, better medication management, and more accurate care delivery. For example, pharmacists can safely review prescriptions, therapists can focus on rehabilitation goals, and nurses can confidently monitor patient progress. The result is better patient care and improved outcomes.
Driving innovation and collaboration
A clear understanding of who HCPs are also helps industries beyond healthcare, including pharma and technology. Pharmaceutical companies engage HCPs for education, research, and clinical trials. Cloud services support HCPs with secure platforms for accessing data. When HCP roles are understood, these collaborations become more effective, fostering innovation that benefits patients and professionals.
Frequently Asked Questions
What is HCP in healthcare?
In healthcare, HCP stands for Healthcare Professional or Healthcare Personnel. It includes all paid or unpaid individuals who provide preventive, curative, or rehabilitative services. This term covers various roles such as physicians, nurses, therapists, pharmacists, EMTs, and social workers in the healthcare industry.
What does HCPs stand for in medical terms?
HCPs is the plural form of Healthcare Professionals. It refers to multiple individuals involved in patient care. It’s important not to confuse HCPs with HCPS, which stands for Hantavirus Cardiopulmonary Syndrome, a severe respiratory illness. The meaning depends on context, especially in medical communication.
Is a HCP a doctor?
A doctor is a type of HCP, but not all Healthcare Personnel are doctors. HCP is a broader term that includes nurses, pharmacists, therapists, physician assistants, dentists, and others involved in patient care within the healthcare workforce.
Further Resources & References
To better understand the role and responsibilities of healthcare personnel (HCPs), several trusted organizations and resources offer valuable guidance. Key industry bodies include the Centers for Disease Control and Prevention (CDC), which provides definitions and infection control protocols specific to HCPs. The World Health Organization (WHO) also outlines global standards for nurses, pharmacists, therapists, and other healthcare workforce members. Regulatory agencies like OSHA and The Joint Commission set compliance requirements to ensure safety in healthcare settings. Surveys such as the Indegene Digital Savvy HCP Survey 2022 and data from the U.S. Bureau of Labor Statistics offer insights into workforce trends and digital engagement.
For reliable, easy-to-understand content about CPR, healthcare practices, and public health education, Simple CPR is here to help. We encourage readers to check out our resources or share this post to support awareness and informed decision-making in the healthcare community.