CPR training is a critical skill, especially to combat any emergency or unexpected situation. With nearly 356,000 out-of-hospital cardiac arrests occurring annually in the U.S., and a staggering ~90% fatality rate, the importance of CPR cannot be overstated (Heart Association, 2023). The difference between life and death often comes down to whether bystanders are trained to act quickly.
Style Snapshot
- Lorem Ipsum is simply dummy text of the printing and typesetting industry.Lorem Ipsum is simply dummy text of the printing and typesetting industry.
- Lorem Ipsum is simply dummy text of the printing and typesetting industry.
- Lorem Ipsum is simply dummy text of the printing and typesetting industry.
- Lorem Ipsum is simply dummy text of the printing and typesetting industry.
- Lorem Ipsum is simply dummy text of the printing and typesetting industry.
- Lorem Ipsum is simply dummy text of the printing and typesetting industry.
Bystander CPR was performed in just 44.7% of out-of-hospital cardiac arrests in 2021, underscoring the need for widespread Heartsaver training (Heart Association, 2024). Whether you’re a layperson or a healthcare professional, proper CPR certification is vital. This article will compare Heartsaver vs BLS, helping you decide which CPR course best suits your needs and goals. Understanding the distinctions between these certifications could be the key to saving a life in a critical moment.
What Is Cardiopulmonary Resuscitation (CPR)?
Cardiopulmonary Resuscitation (CPR) get performed if someone’s heart stops beating or they stop breathing. It combines chest compressions alongside rescue breaths to keep up blood circulation and oxygen supply until professional medical help arrives.
CPR plays a critical role in cardiac arrest situations, as immediate action can double or even triple the chances of survival. CPR helps prevent permanent damage during those crucial minutes before advanced care is available by keeping oxygen-rich blood flowing to vital organs like the brain and heart. Both trained professionals and bystanders can perform CPR, though training improves effectiveness.
Different certification levels, such as Heartsaver vs BLS, address specific audiences. Heartsaver courses are designed for the general public, while Basic Life Support (BLS) is tailored for healthcare providers who require advanced resuscitation skills. Regardless of the training level, CPR is a vital skill that empowers individuals to act swiftly in life-threatening emergencies.
Understanding BLS (Basic Life Support)
Before diving into the details, it’s essential to recognize that Basic Life Support (BLS) builds upon CPR certification by equipping healthcare professionals with advanced lifesaving techniques, teamwork strategies, and medical equipment use- skills that go beyond the scope of Heartsaver CPR or Heartsaver First Aid training.
Definition and Purpose
Basic Life Support (BLS) is an advanced form of CPR designed for healthcare environments. Unlike general CPR certification, BLS emphasizes rapid recognition of cardiac arrest, high-quality chest compressions, and effective use of devices like bag-valve masks. It ensures providers can deliver coordinated care during emergencies, highlighting the difference between the BLS vs Heartsaver cost in training.
Target Audience
BLS is essential for medical professionals and first responders. Physicians, nurses, paramedics, emergency medical technicians, dentists, and hospital staff are typically required to hold active Basic Life Support certification. Unlike Heartsaver CPR courses for the public, BLS is mandated explicitly in healthcare settings where advanced interventions are frequently needed.
Course Content
BLS course material includes adult, child, and infant CPR techniques, plus training in two-rescuer scenarios. Participants learn to use bag-valve-mask (BVM) devices, maintain airway management, and practice effective team dynamics. Compared to Heartsaver First Aid, BLS courses offer broader, advanced skills critical for handling complex emergencies in clinical environments.
Format & Duration
A typical Basic Life Support course lasts 3-4 hours, depending on the delivery format. Options include traditional in-person classes or blended learning that combines online modules with hands-on skills assessments. This flexibility allows busy professionals to pursue CPR certification while effectively managing their demanding healthcare schedules.
Certification & Renewal
BLS certification involves written testing and hands-on skills evaluation to ensure competency. Once earned, certification is generally valid for two years. Renewal requires recertification courses to stay current with the latest guidelines. Compared to Heartsaver CPR training, BLS is more intensive but crucial for maintaining clinical readiness.
Understanding Heartsaver Courses
Unlike Basic Life Support, which is tailored for healthcare providers, the American Heart Association’s Heartsaver programs are designed for everyday people. These courses provide accessible CPR certification and first aid skills, allowing non-medical individuals to step in during emergencies, with training aligned to workplace and community needs.
Definition and Purpose
The AHA’s Heartsaver suite focuses on equipping lay rescuers with essential emergency response skills. Covering Heartsaver CPR, AED use, and Heartsaver First Aid, the courses emphasize prompt action before professional help arrives. Unlike BLS, they focus on simplified techniques suitable for non-clinical environments, often at a lower BLS vs Heartsaver cost.
Target Audience
Heartsaver courses are ideal for teachers, coaches, childcare workers, corporate staff, fitness trainers, and anyone needing CPR certification for workplace compliance or personal preparedness. Unlike Basic Life Support programs for healthcare workers, Heartsaver CPR and First Aid are tailored for individuals without medical backgrounds who still wish to respond effectively in emergencies.
Course Variants
The AHA offers several Heartsaver course options- Heartsaver CPR AED, which focuses on resuscitation and defibrillator use Heartsaver First Aid. It covers injuries, medical emergencies, and environmental concerns. On the other hand, the combined Heartsaver First Aid CPR AED provides comprehensive training. Each course offers practical, simplified approaches compared to Basic Life Support, making lifesaving skills more widely accessible.
Format & Duration
Heartsaver training is flexible and available online, in-person, or in blended formats. Depending on the course, it usually takes 2–5 hours to complete. This versatility makes it convenient for individuals and organizations, offering easier access to CPR certification than the more intensive Basic Life Support courses required in clinical practice.
Certification & Renewal
Certification is awarded after successful skills testing and/or knowledge checks, with cards valid for two years. Renewal is required to maintain an active status and align with updated AHA guidelines. Compared to Basic Life Support, Heartsaver CPR and Heartsaver First Aid certifications are less intensive, but still vital for workplace readiness.
Key Differences Between BLS and Heartsaver
While both programs provide CPR certification, the choice between Basic Life Support and Heartsaver depends on who you are and where you plan to use these skills. Understanding differences in BLS course content, Heartsaver course duration, and healthcare CPR requirements ensures you select the proper training for your professional or personal needs.
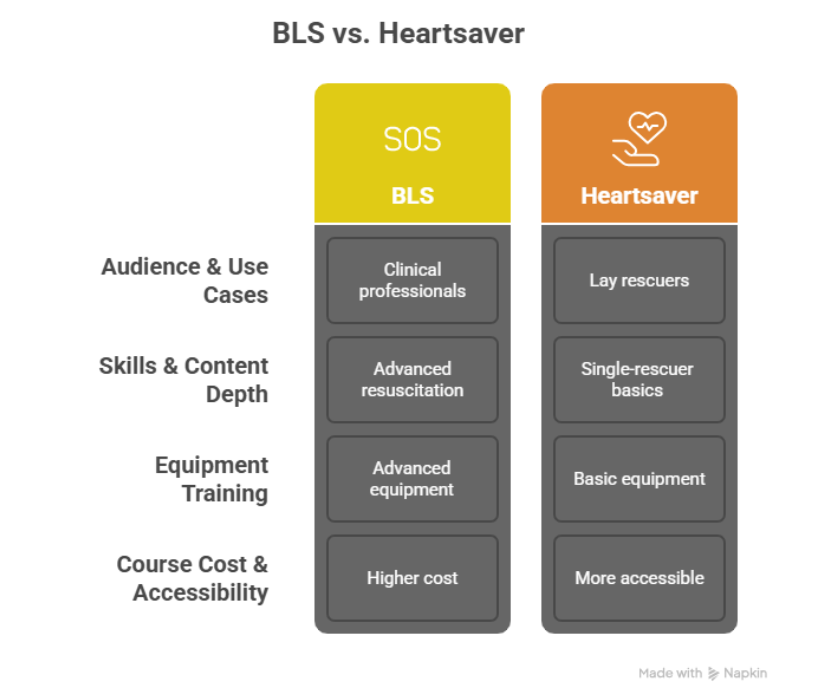
Audience & Use Cases
Basic Life Support is designed for medical professionals and first responders who must meet healthcare CPR requirements in hospitals, clinics, and emergency services. Heartsaver, on the other hand, targets lay rescuers such as teachers, corporate employees, coaches, or caregivers. The primary difference lies in audience and application. BLS is for clinical use, while Heartsaver for public or workplace emergencies.
Skills & Content Depth
BLS course content emphasizes advanced resuscitation skills, such as two-rescuer CPR, airway management, and team-based dynamics. It focuses on delivering high-performance CPR in complex clinical settings. Heartsaver courses, however, concentrate on single-rescuer basics—teaching how to recognize emergencies, perform chest compressions, and use an AED. The training depth differs, reflecting healthcare vs non-medical needs.
Equipment Training
BLS certification involves hands-on practice with advanced equipment such as bag-valve masks (BVMs), emphasizing airway control and coordinated team intervention. By contrast, Heartsaver primarily trains participants on barrier devices like face shields and pocket masks, combined with AED usage. These differences highlight the distinction between professional healthcare CPR requirements and community-focused readiness.
Course Cost & Accessibility
When comparing BLS vs Heartsaver cost, BLS programs are often priced slightly higher because of the advanced skills and equipment training in BLS course content. Heartsaver course duration is generally shorter, making it more accessible to the public. Both are widely available through in-person and blended options, ensuring flexibility for diverse learners.
Which Certification Should You Choose?
Selecting between Basic Life Support and Heartsaver training depends on your career path, workplace standards, and personal goals. By comparing BLS course content, Heartsaver course duration, and specific healthcare CPR requirements, you can make an informed decision that aligns with professional and personal needs.
For Healthcare Professionals
Healthcare workers such as doctors, nurses, and EMTs must complete Basic Life Support training to meet healthcare CPR requirements. The BLS course content emphasizes team-based resuscitation, bag-valve-mask usage, and advanced airway support. Since these skills are essential for hospital and clinical settings, BLS certification remains mandatory for professionals managing life-threatening emergencies daily.
For Non-Healthcare Professionals
For teachers, fitness instructors, childcare providers, or office staff, Heartsaver CPR or Heartsaver First Aid courses are typically sufficient. With a shorter Heartsaver course duration and more straightforward content than BLS, these programs focus on single-rescuer CPR, AED operation, and basic first aid. They provide accessible CPR certification tailored to non-medical roles in community or workplace settings.
For Regulatory/Job Requirements
Specific jobs require CPR certification to meet regulatory standards, such as OSHA compliance for workplace safety. Basic Life Support is the norm in healthcare due to advanced patient care responsibilities, while industries like childcare, fitness, and corporate offices often mandate Heartsaver CPR or Heartsaver First Aid. Choosing depends on the role’s legal and organizational requirements.
For Personal Preparedness
Individuals seeking to protect loved ones at home or respond to emergencies in their community benefit most from Heartsaver training. With flexible Heartsaver course duration and practical skills in CPR, AED use, and first aid, these courses equip everyday people to act confidently in crises—without the advanced focus of BLS course content needed in clinical care.
Frequently Asked Questions
What is the difference between BLS and Heartsaver?
BLS is designed for healthcare professionals, covering advanced CPR, team-based resuscitation, and equipment like bag-valve masks. Heartsaver, by contrast, is intended for lay rescuers and focuses on single-rescuer CPR, AED use, and optional first aid. The choice depends on whether clinical or community-level skills are required.
Can a BLS instructor teach Heartsaver?
Yes, an AHA-certified BLS Instructor can also teach Heartsaver courses. Since BLS is a higher credential, instructors are qualified to deliver Heartsaver CPR and First Aid programs, provided they are aligned with an authorized AHA Training Center and use the approved course materials for proper certification delivery.
Is it better to be CPR or BLS certified?
BLS certification is considered advanced CPR, and it is required for healthcare professionals due to its emphasis on team-based care and advanced techniques. Heartsaver CPR AED is sufficient for laypersons or workplace compliance. The decision depends on your profession, regulatory requirements, and whether you need healthcare-level or general community-level skills.
Is Heartsaver First Aid the same as CPR?
No, Heartsaver First Aid is different from CPR training. It addresses medical emergencies such as bleeding, burns, allergic reactions, and shock, while Heartsaver CPR AED focuses on resuscitation and defibrillator use. Learners may take them separately or combine both for a comprehensive workplace and personal preparedness course.
Trends in CPR Certification
CPR certification has evolved significantly, with blended learning becoming one of the most popular approaches. Programs like HeartCode® for BLS and Heartsaver online courses allow learners to complete theoretical components independently, followed by in-person skills sessions for hands-on practice. This model offers the best of both worlds. Flexibility and reliability are provided for busy professionals through supervised skill testing. Healthcare providers often choose HeartCode® BLS to meet rigorous requirements, while community members benefit from Heartsaver online programs for workplace or personal preparedness. Adopting blended learning reflects modern needs, ensuring broader accessibility and consistency in lifesaving education.
Finding and Registering for a Course
Choosing the right CPR certification program starts with identifying your needs for healthcare CPR requirements or community-level skills. Once decided, learners can easily register online through the American Heart Association or authorized training centers for both BLS and Heartsaver programs.
Online vs In-Person
Online CPR certification offers flexibility, self-paced study, and convenience, but requires an in-person skills test for validity. In-person training ensures immediate feedback, peer interaction, and direct practice under instructor supervision. Classroom-based BLS course content is often preferred for healthcare providers, while lay rescuers may benefit from online or blended Heartsaver course duration options.
Blended Learning Options
Blended courses combine online modules with hands-on practice, ensuring learners know theory before demonstrating skills. This approach saves time, increases accessibility, and allows participants to balance training with work or personal commitments. Both HeartCode® BLS and Heartsaver online use this model for effective certification.
Cost Comparison
BLS vs Heartsaver cost varies by location and provider. Heartsaver courses are typically less expensive, ranging from $60 to $100, while BLS courses cost slightly more due to advanced training. Despite higher fees, BLS offers greater professional value for healthcare providers, while Heartsaver provides affordable and essential certification for the general public.
Wrapping up
Choosing between Heartsaver and BLS depends on your role, responsibilities, and certification requirements. Basic Life Support (BLS) is essential for healthcare providers needing advanced resuscitation skills. At the same time, Heartsaver CPR and First Aid courses empower non-medical individuals to respond effectively in work, home, or community emergencies. Both pathways provide life-saving knowledge, but selecting the right one ensures you meet professional standards or personal preparedness goals.
Ready to earn your CPR certification? Check out flexible, accredited courses with Simple CPR today and get certified online quickly, affordably, and confidently.