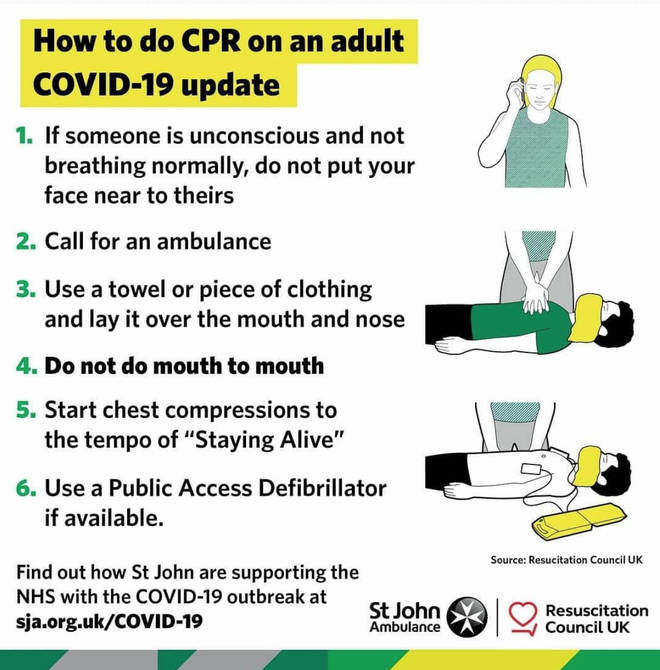
Cardiopulmonary resuscitation stands out as an inherently risky activity in the COVID-19 era: SARS-CoV-2 spreads from person to person through the air, and CPR involves many steps that could aerosolize the virus.
However, healthcare workers and bystanders can take precautions to protect themselves while helping others, as outlined in “interim guidance” recently published in Circulation.
Prior to the pandemic, survival from cardiac arrest had steadily improved thanks to prompt use of measures like chest compression and defibrillation. COVID-19 now requires taking a fresh look at “established processes and practices,” Dana P. Edelson, MD (University of Chicago, IL), and colleagues say. “The challenge is to ensure that patients with or without COVID-19 who experience cardiac arrest get the best possible chance of survival without compromising the safety of rescuers, who will be needed to care for future patients.”
Their practical advice—covering adult, pediatric, and neonatal resuscitations in patients with suspected or confirmed COVID-19 infection, for both in-hospital and out-of-hospital cardiac arrest—arises from a team effort by the American Heart Association (AHA) in collaboration with the American Academy of Pediatrics, the American Association for Respiratory Care, the American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with the support of both the American Association of Critical Care Nurses and National EMS Physicians.
“There’s a reason why we had eight organizations be a part of this. Part of that is because there’s a very small knowledge base right now for how to treat COVID patients and a lot of [that knowledge] is based on things that are literally being published hourly, coming out of China, Italy, France, and other countries,” Comilla Sasson, MD, PhD (University of Colorado Hospital, Denver), told TCTMD. Sasson, who co-authored the document along with 26 other experts, is an emergency medicine physician and the AHA’s vice president for emergency cardiovascular care science and innovation.
“What we tried to do was to take the best-available evidence, for which there is very limited data, combined with what we know from prior infectious disease outbreaks like SARS and MERS, and then really try to figure out [the] delicate balance of making sure that we are trying to optimize patient survival but at the same time being very mindful of exposure risks to providers as well,” she explained.
For the first time, CPR recommendations are calling for clinicians to take a pause and ensure safety before proceeding, Sasson pointed out. “Healthcare providers are a limited, scarce resource, and we have to make sure that their safety is paramount, especially in an infectious disease like this.”
Reduce Exposure, Limit Spread
The document emphasizes three main principles, explaining their rationale and offering specific strategies to achieve them: reduce provider exposure to SARS-CoV-2, prioritize oxygenation and ventilation methods that can lower aerosolization risk, and—for each unique patient and setting—weigh whether it is appropriate to start or continue CPR.
When COVID-19 is a concern, healthcare workers are encouraged to don personal protective equipment prior to initiating CPR and limit the number of personnel present when it occurs. Mechanical CPR devices also can reduce exposure. To limit aerosolization, the right tools can help, such as using a bag-mask device with a HEPA filter and a tight seal; the document also stresses intubation and ventilation of the patient.
Decisions over whether to pursue CPR must be done carefully, though “it is reasonable to consider age, comorbidities, and severity of illness,” according to the guidance.
“Cardiopulmonary resuscitation is a high-intensity team effort that diverts rescuer attention away from other patients. In the context of COVID-19, the risk to the clinical team is increased and resources can be profoundly more limited, particularly in regions that are experiencing a high burden of disease,” Edelson et al observe. “While the outcomes for cardiac arrest in COVID- 19 are as of yet unknown, the mortality for critically ill COVID-19 patients is high and rises with increasing age and comorbidities, particularly cardiovascular disease.”
Importantly, for patients who are COVID-19 negative or aren’t thought to have the disease, “cardiac arrest resuscitations should proceed according to the standard algorithms,” they stress.
Some good news: CPR training is available online. In these uncertain times, it is more important than ever to take measures to insure the safety of your loved ones.
For the entire article, please see the source: https://www.tctmd.com/news/cpr-covid-19-keep-safe-setting-cardiac-arrest